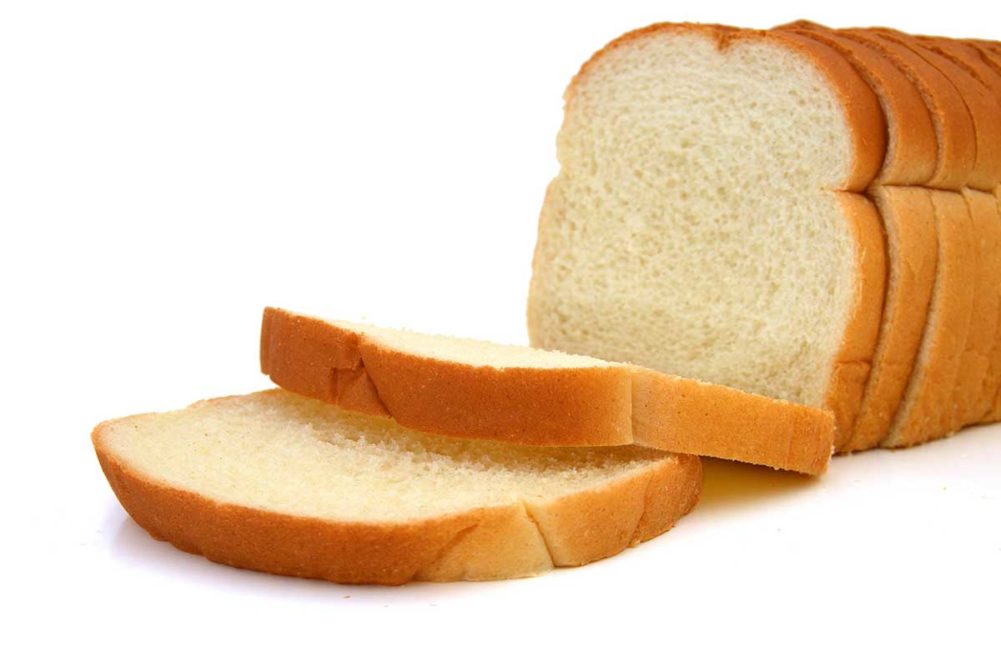
BASEL, SWITZERLAND -- Studying the relationship between intake of 139 foods and nutrients and cancer, researchers said white bread was the only food product found to have a positive association with increased risk of colorectal cancer. Alcohol intake also was found to have a positive association with colorectal cancer (CRC) incidence.
The researchers’ findings were published in Nutrients, Basel, in an article, “Diet-Wide Association, Genetic Susceptibility and Colorectal Cancer Risk: A Prospective Cohort Study.” The paper was written by a team of researchers, led by Dongqing Jin, Department of Colorectal Surgery, The First Affiliated Hospital, Zhejiang University School of Medicine in Hangzhou, China.
Additionally, several nutrients were shown to be negatively associated with the risk of CRC.
“Our results show that higher intakes of alcohol and white bread are associated with increased CRC risk, whilst dietary fiber, calcium, magnesium, phosphorus, and manganese are inversely associated,” the researchers said.
By way of background, the researchers said earlier studies identified red meat and alcohol intake as increasing CRC risk and cereal fiber as reducing risk. The earlier studies did not examine the relationship between a wide range of foods and the disease, they added.
“The purpose of this study was to systematically evaluate the relationship between the 139 foods and nutrients covered in the online questionnaire and the risk of CRC,” the paper said.
For its data, the researchers relied on the UK Biobank, a longitudinal large cohort study of 500,000 middle-aged people recruited between 2006 and 2010 from across the United Kingdom.
“We used baseline information on the population collected by the UK Biobank Assessment Centre and information on cancer status identified through links to national registries,” the paper said. “At the baseline assessment center, a touchscreen questionnaire containing information on socio-demographic characteristics, medical history, and lifestyle factors was issued and standardized anthropometric and biometric measurements were performed. “
The association between CRC incidence and 139 foods an nutrients was measured based on responses to a 24-hour dietary questionnaire completed at recruitment.
Only eight of the foods and nutrients showed a meaningful association. Positive associations were for white bread and alcohol and negative associations were for fiber, calcium, magnesium, phosphorus, manganese and carbohydrate intake.
“There were no significant associations of the remaining foods and nutrients with CRC,” the researchers said.
The researchers offered positive observations about fiber and whole grains.
“Our observational results suggest that dietary fiber is a protective factor for CRC, which is consistent with previous findings,” they said. “Dietary fiber can accelerate intestinal motility, dilute carcinogens in the colon, and ferment fiber into short-chain fatty acids by gut bacteria, all mechanisms that suggest dietary fiber intake may reduce the risk of malignancy and improve colon health. In addition, dietary fiber can be used as a broad pillar of CRC prevention and adjuvant therapy. Although there is a strong mechanism association between fiber intake and CRC risk, epidemiological studies have shown different outcomes between fiber and CRC from different food sources.
“Whole grains, a major source of cereal fiber, are inversely associated with CRC morbidity and mortality. Consistent with previous studies, our results found that high white bread intake was a risk factor for CRC. Notably, whole grains are a major source of many vitamins, minerals, and phytochemicals that have anti-cancer properties and may influence CRC risk through several potential mechanisms.”
The results offer evidence and guidance for the dietary prevention of CRC, the paper said.
“More and larger cohort studies are needed in the future to validate our results and explore more associations between dietary components and CRC risk,” the researchers concluded.
In a letter to investors, the Grain Food Foundation’s executive director Erin Ball said the group’s Scientific Advisory Board had “identified several key issues with the scientific methodology employed.”
“First, the study lacks a hypothesis-driven approach, which is crucial for establishing meaningful correlations,” Ms. Ball said. “Additionally, the reporting primarily focuses on associations, rather than causation, and fails to highlight the multitude of other associations that could be drawn from the same work. The authors of the study appear to have cast a wide net, naming white bread and alcohol as examples without a focused hypothesis.”
Charlotte Martin, a dietitian who works with the GFF as a nutrition consultant, called the study both “insightful and a reminder of the complexities of nutritional science.” At the same time, she too expressed concern about a lack of a “hypothesis-driven methodology.”
“This approach could lead to identifying significant associations purely by chance due to the large number of variables tested,” she said, adding that a reliance on self-reporting makes the study susceptible to inaccuracies.
“The small effect size reported, although statistically significant, also underscores the need for cautious interpretation, particularly in the absence of a clear mechanistic link, as noted with white bread consumption,” Ms. Martin said.
The findings should not “deter individuals from including white bread in their diet in moderation should they choose to,” she said.